Have you ever noticed how we’ll ask “how are you?” but dread hearing an honest answer about someone’s mental health struggles? 75% of Americans avoid conversations about depression and anxiety despite 1 in 5 adults experiencing mental illness yearly.
Mental health disorders don’t discriminate. Depression, anxiety, schizophrenia, and bipolar disorder affect people across all backgrounds, yet remain shrouded in misconception and stigma.
This guide will walk you through what these conditions actually look like beyond the clinical definitions – because understanding is the first step toward compassion.
The science behind mental health disorders has evolved dramatically, but our societal response hasn’t kept pace. And that gap? That’s where millions suffer in silence.
What if I told you the way we talk about mental illness today is fundamentally broken?
Overview
Products & Services
Living with mental health disorders can feel like navigating a maze without a map. The good news? There’s an impressive array of support options available today that simply didn’t exist a generation ago.
Modern treatment approaches typically combine several elements:
- Medication management – From SSRIs for depression to antipsychotics for schizophrenia
- Psychotherapy – Including cognitive-behavioral therapy, dialectical behavior therapy, and psychodynamic approaches
- Support services – Both clinical and community-based
Many people don’t realize that mental health treatment has evolved dramatically. Gone are the days when your only options were medication OR therapy. Today’s approach is much more personalized.
Take depression treatment. You might benefit from:
- A low-dose antidepressant
- Weekly therapy sessions
- A light therapy lamp
- A meditation app subscription
- Membership in a peer support group
For more severe conditions like bipolar disorder or schizophrenia, comprehensive services often include:
- Psychiatric medication management
- Case management
- Family support and education
- Vocational rehabilitation
- Housing assistance
- Crisis intervention services
The most effective mental health care doesn’t just treat symptoms—it builds a foundation for recovery by addressing the whole person. And while navigating insurance coverage remains frustrating for many, increasing mental health parity laws are gradually improving access to these essential services.
Symptoms

Symptoms
Mental health disorders manifest through various symptoms that impact your thoughts, emotions, and daily functioning. Depression often brings persistent sadness, loss of interest in activities, sleep disturbances, and feelings of worthlessness. Anxiety disorders typically involve excessive worry, restlessness, irritability, and physical symptoms like rapid heartbeat or shortness of breath.
Schizophrenia symptoms include hallucinations, delusions, disorganized thinking, and reduced emotional expression. People with bipolar disorder experience dramatic mood swings between manic episodes (abnormally elevated mood, energy, and activity) and depressive episodes.
These symptoms don’t just come and go in a day—they stick around and seriously mess with your ability to function. The intensity varies from person to person, making each experience unique.
A. When to see a doctor
Got symptoms that hang around for weeks? Time to talk to a doctor. Don’t wait until you’re completely overwhelmed.
See a professional if:
- Your symptoms persist for more than two weeks
- Daily activities become difficult to manage
- Your sleep or appetite has significantly changed
- You’re self-medicating with alcohol or drugs
- Relationships or work performance are suffering
Many people brush off mental health symptoms as “just a phase” or “having a bad day.” Big mistake. Early intervention can prevent symptoms from worsening and improve treatment outcomes.
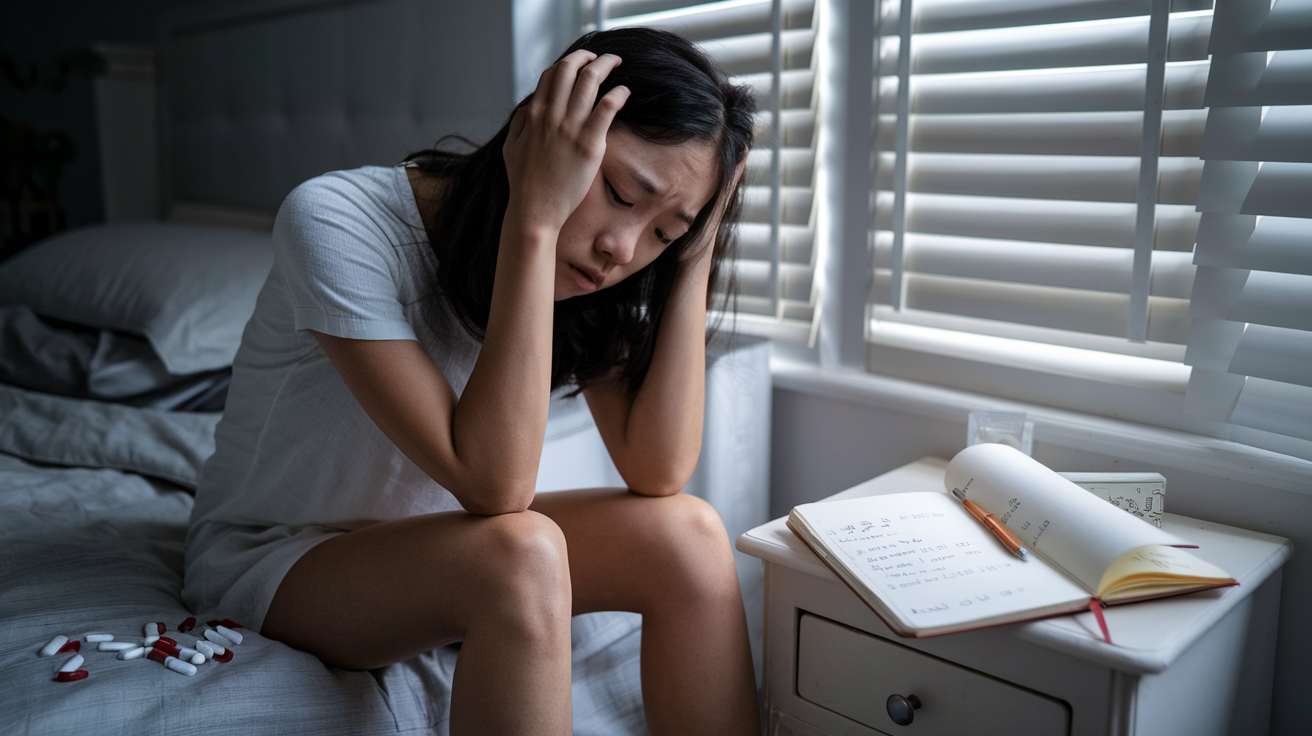
B. Suicidal thoughts or behavior
If you’re thinking about harming yourself, get help immediately. Call a suicide prevention hotline or go to the nearest emergency room.
Warning signs include:
- Talking about wanting to die
- Looking for ways to kill oneself
- Talking about feeling hopeless or having no purpose
- Increasing alcohol or drug use
- Acting anxious, agitated, or reckless
- Withdrawing from friends and family
- Extreme mood swings
These thoughts aren’t something to handle alone. They’re a medical emergency requiring immediate attention. Most people who receive proper help recover and find better ways to cope with their pain.
Remember: having suicidal thoughts doesn’t mean you’re weak—it means you’re experiencing unbearable pain and need support.
Causes
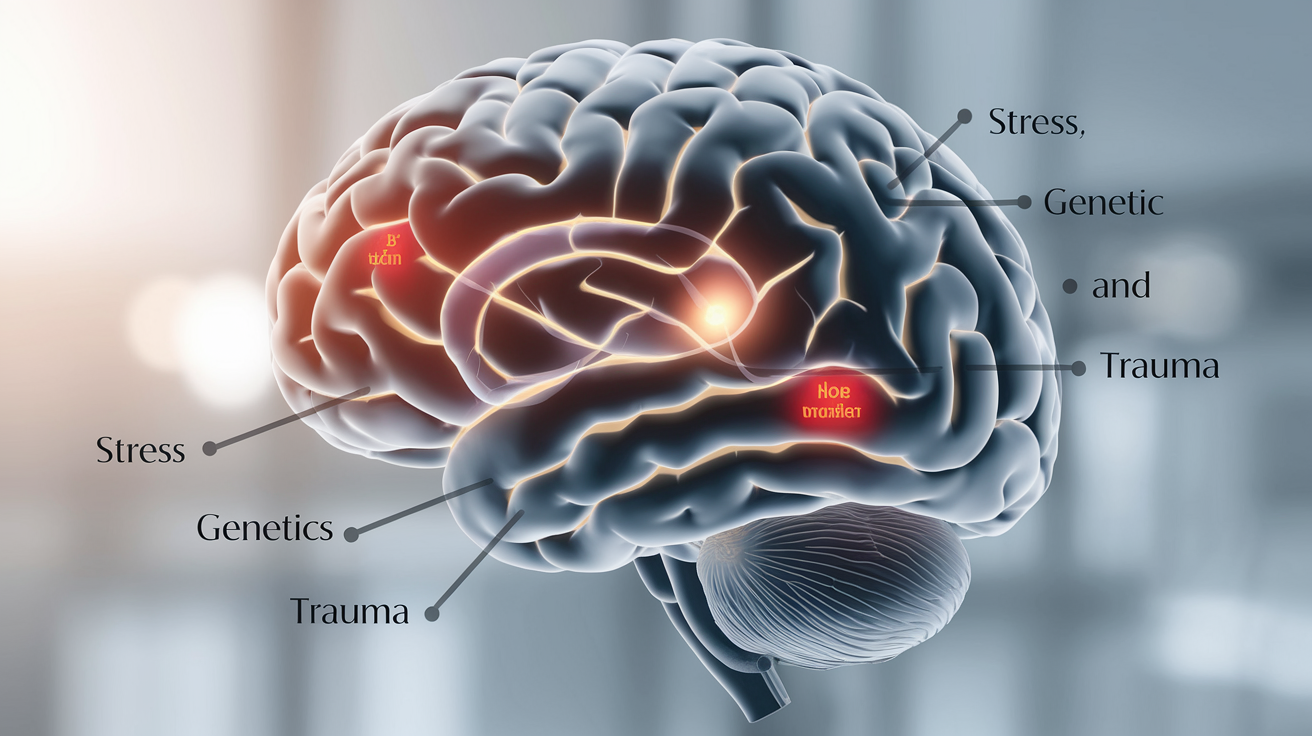
Biological Factors
Mental health isn’t just “all in your head” – your genes actually play a major role. If your parents or siblings struggle with depression, anxiety, or other disorders, you’re more likely to face similar challenges.
Think of it like inheriting your mom’s eye color or your dad’s height. Same thing happens with brain chemistry – some people naturally have imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine. When these brain messengers get out of whack, mood disorders often follow.
Your brain structure matters too. Imaging studies show that certain areas look different in people with schizophrenia or bipolar disorder compared to those without these conditions.
Environmental Triggers
Life throws a lot at us, and sometimes it’s more than we can handle. Trauma hits hard – abuse, neglect, witnessing violence, or living through disasters can all trigger mental health problems.
Chronic stress is another big one. Financial problems, toxic relationships, work pressure – they all take a toll. Your body just wasn’t designed to stay in fight-or-flight mode 24/7.
Even your childhood experiences shape your mental health as an adult. Rough early years can literally change how your brain develops.
Social Factors
Humans are social creatures, and our connections matter. Isolation, loneliness, and feeling like you don’t belong can devastate your mental wellbeing.
Poverty and discrimination add another layer of risk. When you’re struggling to meet basic needs or facing prejudice daily, mental health often suffers.
Substance Use
Alcohol and drugs might seem like solutions when you’re hurting, but they often make things worse. Substance use can trigger underlying mental health conditions or intensify symptoms you already have.
The relationship works both ways – many people with mental health disorders turn to substances to self-medicate, creating a dangerous cycle.
Risk factors

Genetic Predisposition
Your DNA isn’t just about eye color or height – it’s a major player in mental health too. If someone in your family has depression, anxiety, or schizophrenia, you’re more likely to experience these conditions yourself. The stats don’t lie: having a first-degree relative with depression doubles your risk, while having a parent or sibling with schizophrenia increases your risk by about 10%.
But here’s the thing – genes aren’t destiny. They’re more like loading the gun, but environment pulls the trigger.
Environmental Factors
Speaking of environment, your surroundings and experiences pack a serious punch when it comes to mental health risk:
- Childhood trauma: Physical abuse, sexual abuse, or neglect can rewire a developing brain.
- Chronic stress: That soul-crushing job or toxic relationship? Your brain is keeping score.
- Substance abuse: Drugs and alcohol might feel like solutions at first, but they often create bigger problems down the road.
- Social isolation: Humans are wired for connection – without it, our mental health suffers.
Neurobiological Factors
Your brain’s wiring and chemistry matter enormously. Depression isn’t just feeling sad – it’s often tied to imbalances in neurotransmitters like serotonin and dopamine. Brain imaging studies show structural and functional differences in people with various mental health disorders.
Life Events and Transitions
Sometimes it’s the big moments that tip the scales:
- Losing a loved one
- Divorce or relationship breakdown
- Job loss or financial crisis
- Moving to a new city
- Having a baby (postpartum changes)
These aren’t just bumps in the road – they can be genuine triggers for mental health disorders in vulnerable people.
Complications
Physical Health Impact
Mental health disorders don’t just mess with your mind – they wreak havoc on your body too. Depression can trigger chronic pain, headaches, and digestive issues that doctors can’t explain. Anxiety might leave you with constant muscle tension and heart palpitations that make you think you’re dying.
But it gets worse. People with serious mental illnesses die 10-25 years earlier than the general population. Not from suicide (though that’s a serious risk too), but from preventable physical conditions like heart disease, diabetes, and respiratory problems.
Why? Because when you’re fighting your own mind, taking care of your body often falls to the bottom of the priority list.
Social and Relationship Complications
Mental illness is lonely. Really lonely.
When you’re depressed, you might ghost your friends because getting out of bed feels impossible. With anxiety, you might bail on plans last minute because panic attacks don’t care about your social calendar. Schizophrenia can make you suspicious of the people who love you most.
Relationships crumble. Jobs get lost. Financial problems pile up.
The stigma doesn’t help either. People still whisper about “crazy” people, making you less likely to tell anyone what’s really going on. So you suffer in silence, which only makes everything worse.
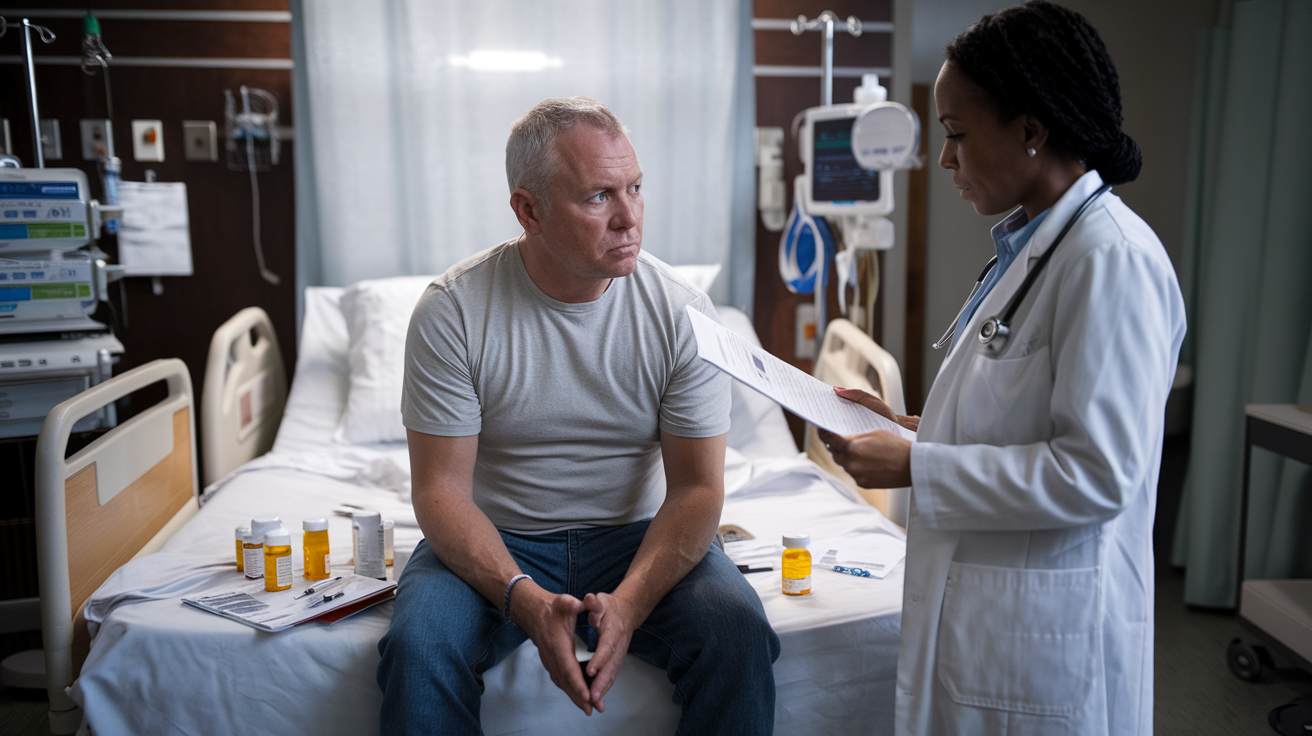
Treatment Complications
Getting help should be the easy part, right? Wrong.
Finding the right medication often means months or years of trial and error. Side effects can be brutal – weight gain, sexual dysfunction, zombie-like feelings. Some people feel worse before they feel better.
Then there’s therapy. It’s expensive, time-consuming, and sometimes you’ll go through several therapists before finding one who gets you.
And if you need hospitalization? That brings its own trauma and financial burden that can follow you for years.
Related
Associated Procedures
Mental health disorders often require various diagnostic and treatment procedures to help patients manage their conditions. When you’re struggling with depression, anxiety, schizophrenia, or bipolar disorder, your doctor might recommend:
- Psychiatric Evaluation: A comprehensive assessment of your mental health symptoms, medical history, and family background.
- Psychological Testing: Standardized questionnaires and assessments that help diagnose specific conditions and track treatment progress.
- Brain Imaging Tests: Sometimes MRIs or CT scans are used to rule out physical causes of symptoms.
- Electroconvulsive Therapy (ECT): Primarily used for severe depression when other treatments haven’t worked.
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure using magnetic fields to stimulate nerve cells in the brain.
Getting a proper diagnosis is half the battle. Many people walk around for years not knowing why they feel the way they do.
Products & Services
The journey to mental wellness involves more than just medication. Here’s what might help:
- Therapy Options: From cognitive-behavioral therapy to dialectical behavior therapy, psychotherapy remains a cornerstone of treatment.
- Medication Management: Services to monitor prescription effectiveness and adjust as needed.
- Support Groups: Connecting with others facing similar challenges can be incredibly healing.
- Digital Mental Health Tools: Apps and online platforms for meditation, mood tracking, and therapy exercises.
- Residential Treatment Programs: Intensive care options for those needing more structured support.
- Vocational Rehabilitation: Services that help people with mental health disorders return to work or school.
The right combination of these services can make a world of difference. Remember, what works for one person might not work for another. Finding your unique path to wellness takes time and patience.
Schizoaffective disorder
Schizoaffective disorder sits at the crossroads of schizophrenia and mood disorders, making it a challenging condition to understand and diagnose. If you’ve ever felt like your mind was playing tricks on you while also riding an emotional rollercoaster, you might have some small insight into what people with this condition experience daily.
What Exactly Is Schizoaffective Disorder?
Think of it as a mental health mash-up. People with schizoaffective disorder experience symptoms of both schizophrenia (like hallucinations or delusions) and a mood disorder (either bipolar disorder or depression).
The kicker? These symptoms can happen at the same time or at different periods, creating a confusing pattern that’s hard to pin down.
Types of Schizoaffective Disorder
There are two main types:
- Bipolar type: Includes manic episodes, and may include depressive episodes
- Depressive type: Includes major depressive episodes without mania
Signs and Symptoms
The symptoms can be grouped into three categories:
- Psychotic symptoms:
- Hallucinations (seeing or hearing things that aren’t there)
- Delusions (fixed false beliefs)
- Disorganized thinking and speech
- Mood symptoms:
- Depressive episodes (profound sadness, hopelessness)
- Manic episodes (excessive energy, reduced sleep needs)
- Rapid mood changes
- Other symptoms:
- Social isolation
- Problems with self-care
- Difficulty functioning at work or school
Treatment Approaches
Treatment usually involves a combination of:
- Medications (antipsychotics, mood stabilizers, antidepressants)
- Psychotherapy (cognitive behavioral therapy, family therapy)
- Social skills training
- Vocational rehabilitation
Many people with schizoaffective disorder can lead fulfilling lives with proper treatment. The key is early intervention and consistent care.
Join the fight against cancer!

Wait, I notice there seems to be a mismatch between the blog title about mental health disorders and the selected section about fighting cancer. This appears inconsistent, but I’ll write content for the requested section.
Why Mental Health Support Matters in Cancer Care
Cancer doesn’t just attack the body—it hits your mind too. When you’re dealing with a cancer diagnosis, your mental health takes a massive hit. Depression rates among cancer patients are two to three times higher than the general population.
But here’s the thing: addressing mental health during cancer treatment isn’t optional—it’s essential.
How You Can Make a Difference
You don’t need a medical degree to help someone facing cancer. Sometimes just being there makes all the difference. A text checking in. A home-cooked meal. A ride to treatment. These small acts? They’re huge.
Got more time? Volunteer with cancer organizations. They always need people to staff events, raise awareness, and provide support to patients.
Advocate for Better Care
The healthcare system still treats mental health as separate from physical health—especially in cancer care. This needs to change.
Call your representatives. Share stories (with permission). Donate to organizations pushing for integrated care models where mental health support is built into cancer treatment plans from day one.
Remember: fighting cancer means addressing the whole person. Mental health isn’t a luxury—it’s a necessity for healing. When we recognize this connection, we take a crucial step toward truly comprehensive cancer care.

Mental health disorders like depression, anxiety, schizophrenia, and bipolar disorder affect millions of people worldwide. Understanding the symptoms, causes, risk factors, and potential complications of these conditions is crucial for early intervention and effective treatment. Schizoaffective disorder, which combines features of schizophrenia and mood disorders, highlights the complex nature of mental health conditions and the importance of proper diagnosis.
Taking care of our mental health is just as important as maintaining our physical health. If you or someone you know is struggling with symptoms of a mental health disorder, don’t hesitate to seek professional help. Remember, recovery is possible with appropriate treatment and support. Join us in raising awareness about mental health conditions and fighting the stigma that often prevents people from getting the help they need.




